The Last-Mile Problem in Healthcare: Can Virtual Clinics Fill the Gap in Rural America?

Introduction: The Last-Mile Problem in Rural Healthcare
When people talk about the “last-mile problem,” they usually mean getting packages from a warehouse to your front door. But in healthcare, the stakes are much higher. In rural America, the last mile can mean the difference between getting timely care or letting a condition worsen. For millions of families, long drives, provider shortages, and unreliable internet stand in the way of basic healthcare access.
So the question is: can virtual clinics solve the last-mile healthcare problem?
The Reality of Rural Healthcare Gaps
Across the U.S., rural communities face some of the deepest healthcare deserts. According to HRSA, about 66.5% of designated primary care Health Professional Shortage Areas (HPSAs) are located in rural (nonmetro) areas, with patients often traveling hours for appointments.
The challenges include:
- Distance: Long travel times, sometimes requiring overnight stays.
- Provider shortages: Declining numbers of rural hospitals and clinics.
- Connectivity gaps: Many households still lack reliable broadband internet.
- Human impact: Patients delay care, miss follow-ups, and rely heavily on emergency rooms for non-emergencies.
From Appalachia, where mountainous terrain isolates communities, to Alaska villages hundreds of miles from the nearest hospital, these challenges are more than an inconvenience. They’re life-altering barriers.
Why Traditional Telehealth Alone Isn’t Enough
Telehealth gained traction during the COVID-19 pandemic, bringing care into homes nationwide. But for rural families, telehealth isn’t always a perfect fit.
- Connectivity limits: Video visits often fail where broadband is scarce.
- Clinical limitations: Standard telehealth can’t capture lung sounds, ear infections, or heart rhythms.
- Trust gaps: Patients want confidence that their remote care matches in-person quality.
That’s why communities are moving beyond standard video visits toward a more sustainable solution: virtual clinics.
Enter Virtual Clinics: A New Model for Rural Access
Virtual clinics are rethinking what healthcare access looks like in underserved areas.
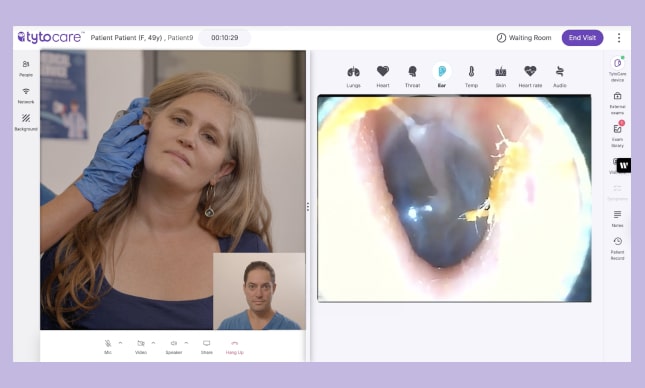
Unlike traditional telehealth, virtual clinics are installed in local hubs like schools, libraries, or community centers. Equipped with devices such as TytoCare’s Pro Smart Clinic, they allow patients to undergo clinical-quality exams guided remotely by a provider.
And with offline-first functionality, exams can be recorded without internet and securely uploaded once connectivity is restored. This makes them especially valuable in communities where broadband is unreliable or unavailable.
Real-World Examples of Virtual Clinics in Action
The model is already transforming healthcare delivery:
- Schools in the Midwest and South have become primary care hubs, where students receive virtual exams without leaving campus.
- Libraries and community centers in states like Nebraska and North Dakota host Pro Smart Clinics, giving residents a trusted, central place to access care.
- Early results show fewer unnecessary ER visits, reduced parent time off work, and better student attendance.
Early results show fewer unnecessary ER visits, reduced parent time off work, and better student attendance. From Appalachia to the Great Plains, virtual clinics are proving they can bridge the last-mile healthcare gap.
How Virtual Clinics Solve the Last-Mile Problem
Virtual clinics address the root causes of rural healthcare inequity:
- Local presence: Care is brought to trusted community sites, reducing travel.
- Offline-first design: Exams don’t stop when the Wi-Fi drops.
- In-person quality, virtually: Clinical-grade exams replicate the experience of being in a doctor’s office.
- Efficient provider reach: One provider can extend care across multiple rural communities.
For rural America, solving the last-mile healthcare challenge isn’t just about convenience. It’s about survival.
Policy and Partnership Potential
Scaling virtual clinics will require collaboration across multiple levels. Fortunately, rural health leaders don’t have to start from scratch. There are existing resources, toolkits, and funding programs designed to help communities take action today:
- Tap into federal and regional support. The HRSA Telehealth Resource Centers offer grants and technical assistance to help rural communities design and implement telehealth solutions.
- Apply for telehealth-specific funding. The Rural Health Information Hub (RHIhub) Telehealth Toolkit includes step-by-step guidance for securing grant dollars and sustaining programs long-term.
- Leverage rural development funds. Programs like the USDA Distance Learning & Telemedicine (DLT) Grant provide funding to deploy advanced telehealth technology in remote communities.
- Use proven partnership frameworks. Guides such as Leveraging Partnerships and Data to Improve Rural Health and Well-Being from the Urban Institute and the Rural Healthcare Investment Playbook from Build Healthy Places Network offer practical models for aligning healthcare, community development, and finance.
- Plan for capital investment. The National Rural Health Resource Center provides a roadmap to capital funding sources and strategies for rural providers.
By connecting health systems, community organizations, and payers with these tools, rural leaders can move beyond identifying the last-mile problem to actually solving it.
Looking Ahead: Virtual Clinics as a Cornerstone of Rural Care
The future of rural healthcare isn’t about patchwork fixes. It’s about a sustainable model that closes the last-mile gap for good.
Virtual clinics won’t replace local providers; they complement them by extending their reach. Together, they offer a blueprint for equitable healthcare: access that doesn’t depend on your zip code.
Conclusion
The last-mile problem in healthcare has persisted for decades. But with virtual clinics, rural America doesn’t have to be left behind. By combining clinical-quality exams, offline functionality, and community-based access, virtual clinics are more than a solution to gaps. They’re redefining what healthcare access can and should look like for everyone.