The ROI of AI in Virtual Care: What Matters to Providers

Introduction: Why ROI Matters in Healthcare AI
Artificial intelligence has become one of the most talked-about tools in healthcare. But while headlines often focus on futuristic possibilities, providers are asking a more practical question: what’s the real return on investment (ROI)?
For providers, ROI in AI-driven virtual care isn’t only about lowering costs or streamlining operations. It’s about improving patient access, reducing clinician burden, and ensuring better outcomes. And just as important: it’s about preserving the human connection that patients value most.
Patients don’t want a future of “automated healthcare.” They want trusted, personal interactions with their clinicians, supported by technology that makes those interactions more effective. The real ROI lies in AI that strengthens, not replaces, the provider-patient relationship.
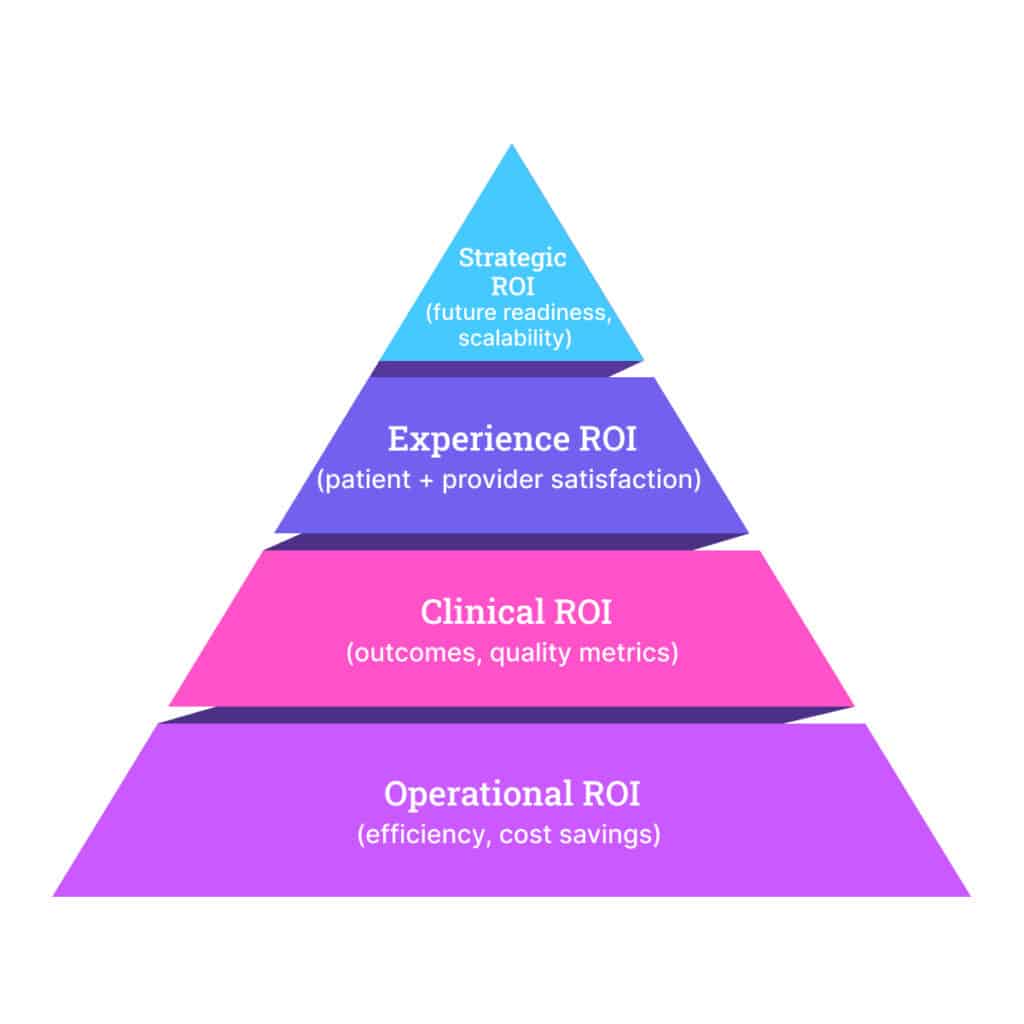
In this post, we’ll explore how providers can think about ROI across four key dimensions: operational efficiency, clinical outcomes, patient and provider experience, and long-term strategic positioning.
Operational ROI: Reducing Burden and Costs
The most immediate value of AI in virtual care comes from operational gains. Health systems face unprecedented staffing shortages and budget constraints, so efficiency isn’t just a “nice to have”; it’s a necessity.
- Clinician workflow efficiency: AI-enabled triage, smart documentation, and automation reduce administrative load, giving clinicians more time to focus on patient care.
- Cost avoidance: By helping patients receive the right level of care virtually, AI reduces unnecessary ED or urgent care utilization.
- Measurable savings: Providers can track metrics such as staff time saved, reduced appointment backlogs, and lower no-show rates.
In fact, a recent survey of U.S. health systems found that AI-enabled virtual care programs delivered a 23% average improvement in efficiency, safety, and staffing impact, a clear demonstration that operational ROI is within reach.
Clinical ROI: Improving Care Quality and Outcomes
While operational savings are important, providers know the ultimate measure of success is patient outcomes.
AI in virtual care supports:
- Early detection and intervention: For example, AI can flag subtle respiratory sounds or irregular heart rhythms during a TytoCare exam, giving clinicians an early warning.
- Readmission reduction: Predictive analytics in remote patient monitoring (RPM) help identify risks before they become acute.
- Quality scores: Better management of chronic conditions and fewer unnecessary escalations can translate into improved quality metrics for health systems.
For providers operating under value-based arrangements, these clinical ROI drivers are just as valuable as financial savings.
Experience ROI: Patients and Providers
ROI also depends on experience, both for patients and for the clinicians delivering care.
For patients, AI-enabled virtual care improves:
- Convenience: Faster access, shorter wait times, and care delivered from home.
- Confidence: The reassurance that their clinician still oversees every interaction.
- Engagement: Proactive outreach and follow-up that keep them connected to their care journey.
For providers, the benefits are equally compelling:
- Reduced burnout: Less time spent on repetitive administrative tasks.
- Job satisfaction: More time to focus on complex cases where their expertise matters most.
- Trust in technology: AI that is explainable, transparent, and supportive builds confidence in both staff and patients.
Experience ROI reminds us that AI isn’t replacing human care. It’s making it more sustainable and meaningful.
Strategic ROI: Positioning for the Future
AI is not just about today’s gains. For U.S. providers, it’s also about staying competitive and aligned with the future of care delivery.
- Scalability: AI-enabled virtual clinics expand access to rural and underserved areas without overextending scarce staff.
- Alignment with payers and policy: CMS and private payers are increasingly rewarding solutions that improve access and outcomes while reducing costs. Providers investing now position themselves to benefit from future reimbursement models.
- Innovation leadership: Early adopters signal to patients, partners, and the market that they are forward-thinking and committed to excellence.
Strategic ROI is about more than technology; it’s about future-proofing healthcare delivery.
Conclusion: What Matters Most
For providers, ROI in AI-driven virtual care is multidimensional. It includes operational savings, clinical improvements, better patient and provider experiences, and long-term strategic advantages.
The bottom line: the most meaningful ROI comes when AI enhances the human side of healthcare. Patients remain at the center, supported, not replaced, by smart technology. For health systems, this means a sustainable path forward: care that is more efficient, higher quality, and more accessible, without sacrificing the relationships that matter most.
As AI matures, providers who measure ROI across all four dimensions will be best positioned to thrive in a healthcare system that is increasingly digital, value-driven, and patient-centered.
FAQs: ROI of AI in Virtual Care
Providers typically measure ROI by tracking operational efficiency (e.g., staff time saved, reduced no-shows), financial savings (avoided ED/urgent care visits), clinical outcomes (reduced readmissions, improved quality scores), and patient/provider experience metrics.
No. Patients want trusted, personal care, and AI is designed to support—not replace—clinicians. The most effective AI solutions handle repetitive tasks, triage, or pattern recognition so that providers can spend more meaningful time with patients.
The key drivers are lower costs through better resource use, improved clinician workflow efficiency, stronger patient engagement, and scalable access to rural and underserved populations.
ROI timelines vary, but U.S. health systems report measurable operational and clinical improvements within the first 12–24 months. Mature programs have shown an average 23% performance improvement across efficiency, safety, staffing, and access, according to Black Book Research.





